Lesson 5: Treatment Defaults In Malaria
Contents
INTRODUCTION:
Welcome to Unit five. In the last unit you learnt about treatment of simple and severe complicated Malaria.
In this unit you will learn about treatment defaults and errors in the management of Malaria and how to manage them. Remember it is very important to know about possible treatment failures so that you can prevent them from occurring or manage them effectively when they occur.
|
By the end of this unit you should be able to:
|
What is Treatment Failure?
Treatment failure in malaria is said to occur when a patient who is diagnosed with malaria fails to improve on a given antimalarial treatment or management plan. Treatment failure should be suspected if a patient deteriorates clinically at any time or symptoms persist 3-14 days after initiation of drug therapy in accordance with the recommended treatment regimen. Development of symptoms 14 days after initiation of therapy where there has been clearance of symptoms should be considered as a new infection and can be treated with the first line drug.
Having seen the definition of treatment failure, let us now turn to factors responsible for treatment failure.
Factors Responsible For Treatment Failure in Malaria Management
Treatment failure in the management of malaria has become quite common in our day-to-day practice.
Before you read on do Activity 5/1, it should not take you more than 3 minutes.
| 1
From your own experience, you may have noticed that some patients fail to respond to malaria treatment. What factors do you think are responsible for this? ………………………………………………………………………………………… ………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ………………………………………………………………………………………………
|
I hope in your answer you mentioned some of the following factors of treatment failure in malaria management:
• Delay in starting antimalarial therapy.
Any delay in starting treatment for malarial infection gives the disease a chance to progress from simple to severe complicated Malaria. Delay in treatment may be caused by health workers who fail to make the correct diagnosis or postpone treatment. Similarly it may be caused by the patient who does not seek medical attention in good time or who fails to take the drugs as prescribed. The latter is quite a common cause of treatment failure in malaria management. As a health worker your role is to start every patient with Malaria on antimalarial treatment without undue delay. Give the first dose if possible under your supervision.
• Incorrect dosages:
Ideally, drug dosages are given per kilogram body weight. Incorrect doses especially under dosing of patients leads to persistence of Malaria infection. This is so because the dose in the body is not sufficient to clear the infection present and hence the disease persists and progresses as the parasites develop resistance to the drug used.
• Failure to elicit a history of recent chemotherapy:
This is another two-sided factor. On the one side, the patient may not volunteer the history of treatment or the medical records of the same. On the other side, the medical worker may due to pressure of work or time limitation fails to elicit treatment history. As a result, your physical examination and laboratory findings may give you information that is misleading or inconsistent. For example, a patient who has taken a single dose of antimalarial treatment 12 hours prior to a blood slide test will return negative results yet the parasites are still alive and kicking.
• Failure to prevent cumulative effects of antimalarial drugs.
All drugs have effects on the normal functioning of the body and antimalarial drugs are no exception. Cumulative effects like nausea and vomiting, hypoglycaemia, haemolysis, and so on, may cause a patient to fail to improve clinically even in the absence of active malaria infection.
• Failure to recognize and treat severe anaemia.
This happens in severely ill patients. When the patient is brought to the health facility we become overwhelmed by the severity of the disease and forget to carry out a basic examination of anaemia. This may lead to fatal results.
• Failure to look for and correct hypoglycaemia
This results in the recurrent convulsions that may be mistaken for cerebral malaria, yet it is hypoglycaemia causing these convulsions.
• Failure to recognize and manage pulmonary oedema, aspiration pneumonia and acidosis.
• Failure to start haemodialysis or peritoneal dialysis.
This is done to correct renal failure in severe Malaria. If not done it could result in fatality hence treatment failure.
• Unjustified withdrawal of an antimalarial drug.
This causes treatment failure because the drug is not given adequate time to act. Some times this happens when the disease progression is fast.
• Failure to switch patients from parenteral to early oral therapy.
This happens in cases where there is a shortage of parenteral medication or where the patient is expected to buy the drugs. As we mentioned in the last unit, it is important to switch your patient from parenteral to oral medication as soon as they stabilize and can take it orally.
• Failure to review antimalarial treatment in a patient whose condition is deteriorating.
This is quite common when the patient is being managed for simple malaria as an outpatient. Such patients are expected to keep their review appointments so that they can be followed up. If they don’t, then treatment failure may occur.
• Multiple diagnoses on a patient.
Multiple diagnoses may cause a health worker to concentrate on one disease at the detriment of the other. If the other disease is malaria then treatment failure may result. The health worker may also miss out on the diagnosis for malaria and hence cause the patient to deteriorate.
• Substandard drugs
When a patient is treated with drugs of poor quality or those that have a low drug content, he or she can not get cured. Even if such drugs are administered in the right number they cannot cure malaria even if the parasites are not resistant. In some cases the drugs have a low dissolution rate thereby resulting in suboptimal therapeutic levels.
• True drug resistance.
There is increased resistance of P. falciparum malaria to chloroquine and fansidar (SP). This is as a result of misuse of these antimalarials in the community. It may also be as a result of emergence of a resistant P. falciparum strain. The malaria parasites are resistant to the drug and even if the drug is good quality and is administered correctly, the disease cannot be cured.
• Others include failure to:
Control convulsions; recognize minor convulsions; and delay in considering obstetric intervention in late pregnancy.
Having looked at the common causes of treatment failure, let us now consider the errors that occur in the management of malaria.
Errors In Managements of Malaria.
Malaria, especially severe complicated Malaria is an acute medical emergency. A patient with severe complicated malaria should therefore be managed as follows:
- Admission in an intensive care unit;
- Be under care of an adequate number of well experience and equipped nurses;
- Be under the close supervision of a clinician and nursing staff;
- Have all observations properly recorded;
- Follow a strict drug administration.
Because of the complexity of all the above protocol, some errors do occur in the management of Malaria. What do we mean by errors? We are here referring to the commission or omission of something in the process of treatment that may result into treatment failure or a poor outcome.
Before you read on, do activity 2, it should take you 3 minutes to complete.
| 2
What are the common errors in the management of Malaria that you have noticed in your health facility? ………………………………………………………………………………………… ………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ………………………………………………………………………………………………
|
Now read the following section and check how many of these errors you were able to state.
Some of the common errors in the management of malaria include:
- Inappropriate route and schedule of antimalarial administration;
- Erratic cessation of treatment;
- Inadequate nursing care;
- Errors in fluid and electrolyte replacement;
- Use of inappropriate drugs e.g. Chloroquine alone in areas with high chloroquine resistance;
- Over treatment or overdose;
- Unnecessary endotracheal intubations;
- Use of potentially dangerous ancillary drugs such as steroids;
- Failure to pass Nasogastric tube to prevent aspiration and for feeding;
- Failure to cover with antibiotics if the decision is taken to delay lumber puncture.
|
Do any of these errors occur in your health facility? DO NOT RISK THE LIFE OF YOUR PATIENTS DO THE CORRECT THING. |
Having learnt about the errors that can occur in the management of Malaria, let’s now see how we can prevent them.
Prevention of Treatment Failures and Errors in Malaria Management
It is a common saying that prevention is better than cure! You as a health worker therefore have the responsibility to make sure these treatment failures and errors do not occur in our practice and in the communities.
Before you read on do activity 3, it should take you about 5 minutes to complete.
| 3
The management of treatment failures and errors is both costly and time consuming. How can you prevent them from occurring? ………………………………………………………………………………………… ………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ………………………………………………………………………………………………
|
Confirm your answer as you read the following discussion.
There are a number of things we need to adopt and apply in our daily practice in order to prevent treatment failures and errors in malaria management. These are:
- Making proper diagnosis and start the appropriate treatment without any delay.
- Prescribing and administering drugs according to body weight or as directed by the manufacturer, or using treatment guidelines from the Ministry of Health;
- Always weighing your patients, especially children;
- Using the correct dosages over the recommended time period;
- Continuously monitoring the progress and treatment of your patient to avoid cumulative effects of antimalarials;
- Doing a thorough examination of the patients and carrying out all the investigations needed;
- Stabilising all your patients, i.e., correcting hypoglycaemia, controlling convulsions, safeguarding the airway, correcting dehydration, acidosis and controlling the temperature;
- Treating any complications that arise in a timely manner, e.g., dialysis for renal failure, blood transfusion for severe anaemia etc;
- Always excluding all possible differential diagnosis;
- NOT withdrawing drugs without just cause;
- Reviewing all your treatment especially when the patient is not showing good response or when patient is deteriorating;
- Starting all patients able to take and tolerate oral medication on oral drugs;
- Using the drugs recommended by the ministry of health according to the resistance pattern observed in your area;
- Considering the appropriate obstetric intervention in late pregnancy in pregnant mothers;
- Providing adequate nursing care;
- Using oral and I/V fluids appropriately depending on the demand and fluid balance of the patient;
- Ensuring that we do not over treat , overdose or under dose our patients.
- Not using potentially dangerous ancillary drugs such as steroids;
- Taking the appropriate action whenever considering adequate treatment and the use of antibiotics.
Next, let us consider the management of treatment failures and errors in malaria treatment.
Management of Treatment Failures and Errors in Malaria Treatment
The following are some of the ways to manage treatment failures and errors in malaria treatment:
- Using the appropriate antimalarial drugs for the treatment of Malaria;
- Administering the drugs for the correct period and schedule to ensure the dose is completed as recommended.
- Re-evaluating all patients who are not responding to treatment appropriately and changing the treatment as deemed necessary.
- Assessing, investigating and excluding all possible differential diagnosis in a patient with malaria and treating all the concurrent diseases appropriately.
Before you read on do activity 4, it should take you 3 minutes to complete.
| 4
Have you come across the term “pharmacovigilance”? Outline the three methods used to monitor the safety of medicines. ………………………………………………………………………………………… ………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ………………………………………………………………………………………………
|
Now read the following section and check how many methods you were able to state.
Medicines are essential chemical compounds, which when administered interact with the body system resulting in some reaction or event. Pharmacovigilance is a term commonly used both by academicians, regulators and workers in the drug industry. It is the science and activities relating to the detection, assessment, understanding and prevention of adverse effects of medicinal products or any other drug-related problems. It is often considered equivalent to post marketing surveillance, although according to the current medicines safety regulations it covers a wider area. Pharmacovigilance represents the continued surveillance of a marketed medicine to assure that the clinical justification is fulfilled continuously during the marketing life of the drug. It promotes rational and safe use of Medicines
The following methods can be used for checking if drugs on the market fulfil their intended role in society. In other words, to check if resources spent on drugs produce optimal results in terms of alleviating human suffering and reducing disease related to economic loss. These are:
• Active surveillance system. This involves collecting case safety information as a continuous pre-organized process;
• Clinical trials. Systemic studies on pharmaceutical products in human subjects (including patients and other volunteers) in order to discover or verify the effects of and/or identify any adverse reaction to investigational products. They also study the absorption, distribution, metabolism and excretion of the products with the objective of ascertaining their efficacy and safety. Clinical trials are generally classified in four phases, as follows:
- Phase I - Healthy volunteers (20 – 50)
- Phase II - a few patients (150 – 350)
- Phase III - more patients 250 – 2000) and
- Phase IV - for approved indications after registration and marketing
• Post market Drug surveillance: This involves carrying out a post market analysis of the quality of drugs, which are available in the market after the registration process.
Conducting Clinical Therapeutic Efficacy Tests
Since the resistance to chloroquine was reported in 1979 in East Africa, the development of resistance to other antimalarials has also become widespread. Countries have had to change or develop new rational antimalarial drug policies using drugs of proven efficacy. Each country is required to build the capacity of staff at the district level to enable them obtain the necessary clinical evidence for its antimalarial drug policy, through conducting therapeutic efficacy tests.
| 5
Outline the standard protocol for monitoring efficacy of antimalarial drugs for treatment of uncomplicated falciparum malaria ………………………………………………………………………………………… ………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ………………………………………………………………………………………………
|
- A research protocol will be written.
- Appropriate sample size of patients will need to be followed for 28 days.
- Regular blood smears will need to be taken on days 0, 3, 7, 14 and 28.
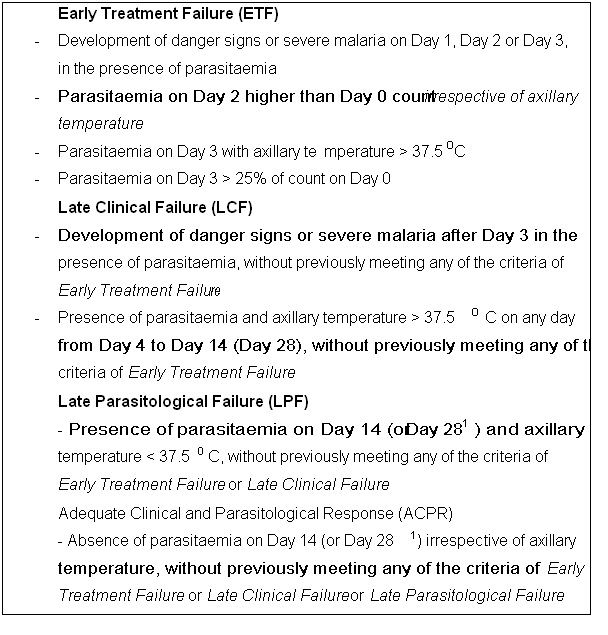
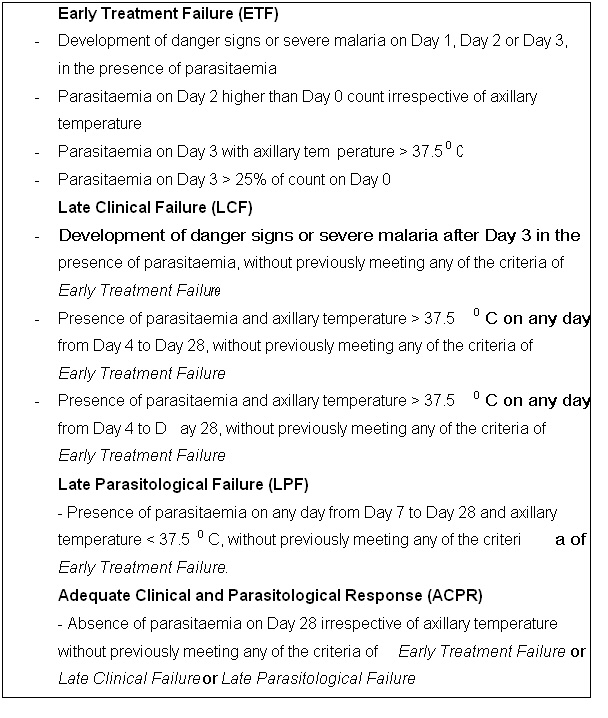
- After the study the patients will be classified as the end points e.g. early treatment failure
(ETF), Adequate Clinical Clinical and Parasitological Response (ACPR) or Late Treatment Failure (LTF)
The section below should first address the protocol for monitoring antimalarial drug efficacy and then finish by summarising the outline or contents of the report
SAMPLE TABLE OF CONTENTS OF A PROTOCOL FOR MONITORING EFFICACY OF ANTIMALARIAL DRUGS
COVER PAGE: :Title, Principal investigator, Co-investigators, Performing nstitution, Study Site, expected start and completion dates and Sponsor
BACKGROUND: :Malaria situation in the country and previous studies on drug Resistance
OBJECTIVES::General and Specific
STUDY DESIGN: :Description of the site, timing, composition of team, drugs to be tested (antimalarial drugs, concomitant treatment, rescue treatment).
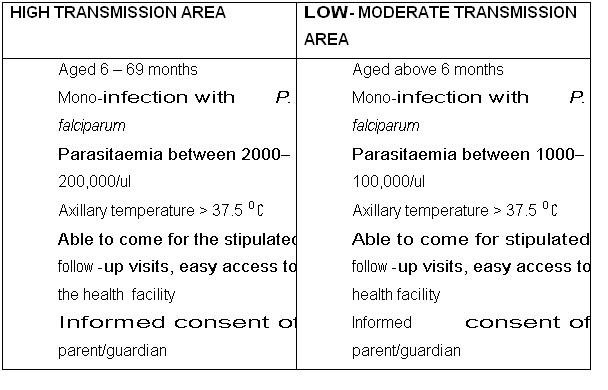
INCLUSION CRITERIA:
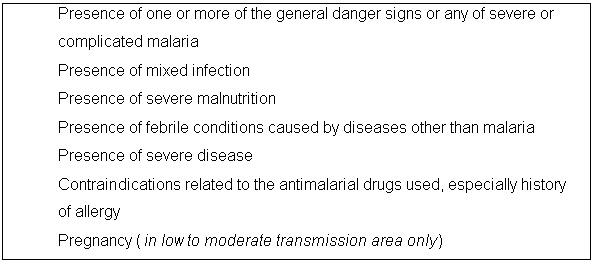
EXCLUSION CRITERIA:
SAMPLE SIZE:
Estimation of the population proportion should be determined at a confidence level of 95%
SCREENING AND ENROLMENT PROCEDURES
- ETHICAL ISSUES
- Approval by ethical committee
- Informed consent
LABORATORY EXAMINATIONS
- Blood smear for malaria diagnosis
- Haematological assessment (haemoglobin/haematocrit) (Optional)
- Urinary test (Optional)
- PCR (mandatory in high transmission area if 28-day follow-up)
- Pregnancy test (if adults included)
END POINTS
- All patients must be classified as Adequate Clinical and Parasitological Response ACPR), Late Parasitological Failure (LPF), Late Clinical Failure (LCF) Early Treatment Failure (ETF), Loss to Follow-up (LF) or withdrawn (W).
High transmission areas
1 If 28-day follow-up
Low to moderate transmission areas
Reasons for withdrawal of a patient from the study, including voluntary and involuntary withdrawal and protocol violation
- Withdrawal of consent
- Failure to complete the treatment
- Persistent vomiting of the treatment
- Severe side-effects necessitating hospitalization
Occurrence during the follow-up of concomitant disease that would interfere with a clear classification of the treatment outcome
- Reinfection with P. falciparum during the follow-up
- PCR unclassifiable results
- Detection of another malaria species infection during the follow-up
- Antimalarial (or antibiotics with antimalarial activity) treatment administered by a third
party or self-medication with antimalaria (or antibiotics with antimalarial activity)
- Failure to attend all the scheduled visits
- Erroneous inclusion of a patient outside of the inclusion/exclusion criteria
- Severe malaria occurring at Day 0
- Misclassification of a patient due to a laboratory error (parasitaemia) leading to the administration of the rescue treatment
Reports from prescribers, researchers and antimalarial drug users are indicating dissatisfaction with the current antimalarial treatment policy. Evidence from clinical efficacy studies show that the antimalarial drugs recommended in the policy for treatment of uncomplicated malaria are failing. Describe the process for changing the antimalarial drug policy.
| 6
Describe four steps for changing and developing a new antimalarial drug policy. ………………………………………………………………………………………… ………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ………………………………………………………………………………………………
|
We hope your answer included the following steps that need to be put in place when changing an antimalarial drug policy. These are:
- Constitute an antimalarial drugs Technical Working Group (TWG);
- Provide evidence of clinical antimalarial efficacy data;
- Select the alternative suitable antimalarial drug;
- Determine safety profile of the drug;
- Determine the cost of the drug;
- Dose regimen and compliance;
- Formulations available;
- Suitability for various and special groups;
- Adverse reaction/event;
- Develop a system for pharmacovigilance.
CONCLUSION
Bravo! You have now come to the end of this unit. In this unit we discussed treatment failures and errors in the management of malaria. We saw that most of these failures and errors are a result of wrong practices by both the community and health workers. We also learnt the importance of identifying and correcting treatment failures promptly and the various ways we can prevent them from occurring. Our role as health workers is therefore to make sure our patients get proper treatment for Malaria.
You should now go back to the beginning of this unit and review the objectives we set out there. If there are any you are not sure about review the necessary section again. If you feel confident that you have achieved all of them complete the attached Assignment before you proceed to next unit. Make sure you also do the practical exercise below to reinforce your knowledge and skills in the management of malaria.
THINGS TO DO IN THIS UNIT
Send your findings to the tutor together with your assignment. |
GLOSSARY
Adverse reaction:
- A response to a drug which is noxious andunintended, and which occurs at doses normally used in man for the prophylaxis, diagnosis, or therapy of disease, or for the modifications of physiological function and the intervention by another drug (antidote) is necessary.
Adverse event:
- Medical occurrence temporarily associated with the use of a medicinal product, but not necessarily causally related. Unexplained occurrence.
Side effect:
- Unintended effect occurring at normal dose related to the pharmacological properties. The use of the drug hould be stopped.
Pharmacovigilance:
- The science and activities relating to the detection, assessment, understanding and prevention of adverse effects of medicinal products or any other drug-related problem.
|
AMREF DIRECTORATE OF LEARNING SYSTEMS
Student Name __________________________________ Student Number:_________________________________ Student Postal Address: __________________________ __________________________
DISTANCE LEARNING COURSE ON MALARIA
Unit 5: Treatment Defaults in Malaria
………………………………………………………………………………………… ………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… 3. Give at least 10 ways of preventing treatment failures. ………………………………………………………………………………………… ………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… 4. List the six end points of antimalarial drug sensitivity outcome to which all enrolled patients must be classified. ………………………………………………………………………………………… ………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… ……………………………………………………………………………………………… ………………………………………………………………………………………………
………………………………………………………………………………………… ………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… 6. What do you understand by the term pharmacovigilance? ………………………………………………………………………………………… ………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… Congratulations! You have come to the end of this assignment. Post it or bring it in person to AMREF. If you have experienced any problems in this unit or assignment, please write to us. Your tutor will be happy to give you relevant responses to enable you cope with the course. Time spent doing the assignment: Hours …………………. Minutes ………….. |