Lesson 2: Integrated Management of Childhood Illness (IMCI)
Contents
INTRODUCTION
Welcome to the second unit of the child health course. In this unit we shall discuss the IMCI strategy which was launched by WHO and UNICEF in 1995. We shall discuss the aims of this strategy, its various components and targets. We shall also look at the list of IMCI recommended drugs. This unit gives general highlights of this strategy. In order to be proficient in IMCI case management , you will need to visit the hospital to learn the practical aspects of IMCI case management and see for yourself how the first component of this strategy is implemented.
Let us now look at the objectives of this unit.
|
By the end of this unit you should be able to:
|
2.1 WHAT IS THE IMCI STRATEGY?
| 1
Before you read on please do the following activity. Have you heard about the IMCI strategy? If yes, briefly write down what you know about it …………………………………………………………………………………………………………………… …………………………………………………………………………………………………………………… …………………………………………………………………………………………………………………… ……………………………………………………………………………………………………………………
|
This is an innovative approach which was started in 1995 by WHO and UNICEF with the aim of introducing a comprehensive and timely management of the 5 most common causes of ill health and death among the under-fives. These illnesses are:
- Pneumonia;
- Diarrhoea;
- Malaria;
- measles;
- malnutrition.
2.2 WHY DO WE NEED TO HAVE AN INTEGRATED APPROACH?
The evidence that a large proportion of childhood morbidity and mortality in the development world is caused by just five conditions is really not enough justification for an integrated approach. However, most sick children present with signs and symptoms related to more than one of these conditions. This overlap means that a single diagnosis may neither be possible nor appropriate (see Table 1.1). Treatment of childhood illness may also be complicated by the need to combine therapy for several conditions. An integrated approach to managing sick children is, therefore, indicated, as is the need to go beyond single diseases and address the overall health of a child.
Therefore, the IMCI strategy combines improved management of childhood illnesses with aspects of nutrition, immunization, and several other important influences on child health, including maternal health. The IMCI strategy aims at reducing death, and frequency and severity of illness and disability, by integrating treatment and prevention of major childhood illnesses, to contribute to improved growth and development.
Table 1.1 Diagnosis of common childhood diseases
For many sick children a single diagnosis may not be apparent or appropriate.
| Presenting complaint | Possible cause or associated condition |
|---|---|
| Cough and / or fast breathing | Pneumonia
Severe anaemia P.Falciparum malaria |
| Lethargy or unconsciousness | Cerebral malaria
Meningitis Severe dehydration Very severe pneumonia |
| Measles rash | Pneumonia
Diarrhoea Ear infection |
| Very sick young infant | Pneumonia
Meningitis Sepsis |
Having discussed the origin and aim of the IMCI strategy, let us know look at its components.
2.3 COMPONENTS OF THE IMCI STRATEGY
Before you read on, do the following activity. It should take you 3 minutes to complete.
Compare your answer with the information given in the following discussion. The IMCI Strategy has 3 components. These are:
- Improvement of health worker skills.
- Improvement of health systems
- Improvement of family and community practices
For IMCI to make an impact, the above three components must go together in tandem. This means that at least 60% of health workers who manage under-fives in 80% of our health facilities are trained in IMCI case management. The health systems are working and community and family practices have been improved. Trained health workers must also be supervised to reinforce their skills.
Let us look at each component in turn.
1. Improvement of Health Worker Skills.
This takes the form of training in the case management of sick children. In Kenya, the Division of Child Health at the Ministry of Health has trained facilitators and provincial health management teams on the case management training for health workers.
IMCI Case Management
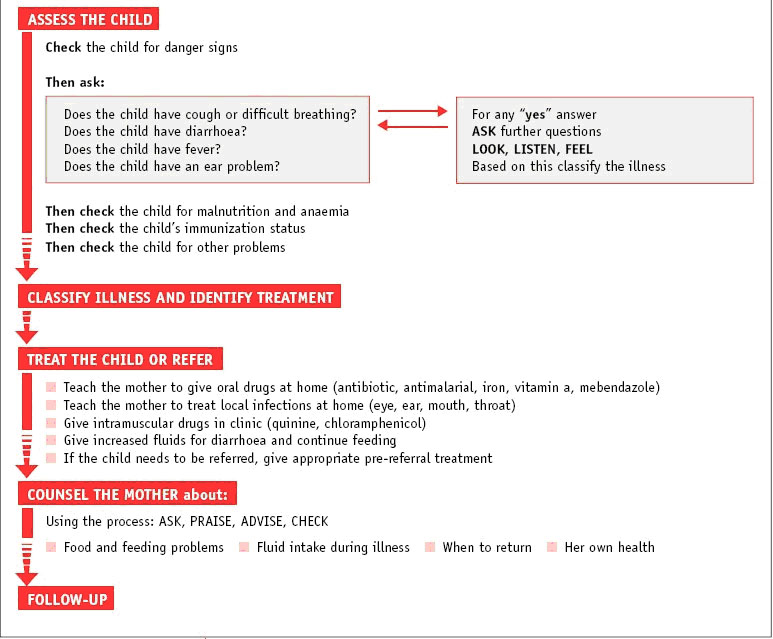
IMCI case management requires you to have a well-defined set of knowledge and skills so that you can accurately assess, classify, and treat ill children and, thereby, reduce mortality and avert significant disability (Figure 2.1). Case management relies on case detection using simple clinical signs and empirical treatment. As few clinical signs as possible are used; these signs strike a careful balance between sensitivity and specificity.
Figure 2.1: IMCI Case management: Source: WHO/CHS/CAH/98.1EREV.1 1999
The complete IMCI case management process involves the following:
- The health worker assesses a child by checking first for danger signs, asking questions about common conditions (cough or difficult breathing, diarrhoea, fever, and ear problems), examining the child, and checking the nutrition and immunization status. The health worker also assesses the child for other health problems.
- The health worker classifies a child’s illnesses using a classification chart. Many health workers are familiar with this system from experience with the WHO case management guidelines for diarrhoea and acute respiratory infections. Because children often have more than one condition, the health worker classifies each illness according to whether it requires urgent pre-referral treatment and referral, specific medical treatment and advice, or simple advice on home management.
- After classification, the health worker identifies specific treatments and develops an integrated treatment plan for each child. If a child requires urgent referral, the health worker gives essential treatment before the patient is transferred. If a child needs treatment at home, the health worker
- gives the first dose of drugs to the child.
- The health worker provides practical treatment instructions, including advising the caretaker on how to give oral drugs, how to feed and give fluids during illness, and how to treat local infections at home. The health worker asks the caretaker to return for follow-up on a certain date, and teaches them how to recognize signs that indicate that the child should return immediately to the health facility.
- If a child is underweight, the health worker identifies treatment or refers the child, when appropriate. The health worker also provides counselling to solve feeding problems, including assessment of breastfeeding practices. If a child should be immunized, the health worker gives immunizations.
- When a child is brought back to the clinic as requested, the health worker gives follow-up care and, if necessary, reassesses the child for new problems.
Remember, in order to apply IMCI case management process properly you need to learn the skills from a trained IMCI facilitator.
Attached to this unit, is the IMCI chart booklet. This booklet gives guidelines on the following:
- assessment,
- classification,
- identification of treatment of sick under fives and
- treatment
- Counselling of caretakers.
I am sure you have seen posters with these guidelines in your health facility. It is important to have these guidelines nearby so that you can apply them correctly in the management of childhood illnesses in your health facility.
Various modes of training health workers in IMCI have been adopted by the MOH. These include:
- Regular 11 day training as stated above.
- On job training. This is done in a health facility by a trained health worker transferring skills to untrained colleagues. This is the method you should use to acquire skills by learning from someone already trained.
- Distance learning using computer based training modules. When taking a distance learning course, you will still need to contact the person in charge of IMCI in the district headquarters or in your hospital to help you acquire practical skills on IMCI case management.
During this training, health workers are taught how to assess children using the IMCI strategy.
How do we assess children using IMCI strategy?
In IMCI we assess children for a number of things:
1. In IMCI all children are assessed first for the following danger signs:
- lethargic or unconscious
- Convulsing now
- History of convulsions
- Vomiting everything
- Not able to drink or breastfeed
If you find a child with any of these danger signs, you should managed them quickly and if necessary refer after giving them pre-referral treatment.
2. After the danger signs, children are then assessed for four main symptoms. These are:
- Cough and difficult breathing
- Diarrhoea
- Fever
- Ear problem
3. Following these, all children are assessed for malnutrition and anaemia, and for possible HIV infection.
4. Finally all children’s immunization and vitamin A supplementation status is checked. Any missed vaccines are given for children who do not have severe classifications.
This is explained further in Charts 1 to 6 which are attached at the end of this Unit as Appendix 1.
The next component of IMCI is the improvement of health systems. Before we embark on this discussion, please do the following activity.
| 3
Before you read the next section, please answer the following questions. 1. Does your facility have a list of essential drugs? …………………………………………………………………………………………………………………… ……………………………………………………………………………………………………………………
…………………………………………………………………………………………………………………… ……………………………………………………………………………………………………………………
…………………………………………………………………………………………………………………… ……………………………………………………………………………………………………………………
|
Check your answers as you read the following discussions.
2. Improvement of Health Systems
The IMCI strategy requires that the health system is strengthened to support the strategy in the following ways:
- Ensuring the availability of essential drugs and supplies.
- Organization of the hospital emergency area to support rapid evaluation and management of sick children.
- Training of health workers in Emergency Triage Assessment and Treatment(ETAT)
- Adherence to National policies for standards of care
- Availing job aides in critical areas
The following table gives a list of drugs that are considered to be essential and should be available in the health facilities.
Table 2.2: LIST OF ESSENTIAL IMCI RECOMMENDED DRUGS
| NO. | DRUG |
|---|---|
| 1. | Artemether/Lumefantrine |
| 2. | Amodiaquine Tabs (200mg) |
| 3. | Quinine (inj.) (vials) (600mg/2ml) |
| 4. | Amoxycillin Tabs (250mg)/syrup 250 mg or 125/5 ml |
| 5. | Chloramphenical (inj) 1g vials |
| 6. | Chloramphenical syrup (600ml bottles) 125mg/5mls |
| 7. | Gentamicin (vials (80mg/2ml) |
| 8. | Crystalline penicillin 100,000 units vials |
| 9. | ORS 500ml sachet |
| 10. | Hartmanns solution 500ml bottles |
| 11. | Nalidixic acid (250mg tabs) |
| 12. | Metronidazole (200mg tabs) |
| 13. | Erythromycin (250mg tabs) |
| 14. | Mebendazole 500 mg tabs |
| 15. | Iron 200mg |
| 16. | Cotrimoxazole (80mg:400mg) |
| 17. | Folic Acid tabs (5mg) |
| 18. | Paracetamol tabs (500mg) |
| 19. | Gentian Violet |
| 20. | Mycostatin (20ml) |
| 21. | Diazepam – vials |
| 22. | 10% glucose ½ litre bottle |
| 23. | Salbutamol (tabs) 2mg |
| 24. | Salbutamol inhaler |
| 25. | Salbutamol nebulization solution (50ml bottle) |
| 26. | Vitamin A (capsules) soft gelatmous 100,000 and 200,000 units |
| 27. | Essential Non pharmaceuticals |
The next critical step in this component of IMCI is the organisation of the hospital emergency area to support rapid evaluation and management of sick children. Let us briefly look at how this should be done.
Organisation of Hospital Emergency Area
As you are well aware, district, sub-district and provincial hospitals act as referral centres for peripheral health facilities. It is therefore critical that their emergency area is organized to respond to the needs of sick children. The following are important points in the organization of an emergency receiving area:
- Triage of sick children should be done by a designated person who may be a health worker, records clerk or even a trained guard. Triaging is a system of sorting out or identifying sick children who need urgent attention so that they can receive prompt management. It can save a life.
- Essential emergency drugs e.g. anticonvulsants, dextrose, oxygen; bronchodilators must be available at all times. These should be accessible without the patient having to pay first;
- Essential supplies like cannulas, ambu bags, oxygen delivery equipment should be available;
- Critically ill children must be attended to without having to undergo registration or any such formality that can cause a delay;
- Newborn babies should not be made to wait in queues.
- Referrals should always be seen urgently
The following two case studies with activities amplify why we need to organise our emergency area to respond to emergencies.
| 1
Kazungu a 7 year old boy was taken to a health centre because of diarrhoea and vomiting which had started that morning. At the facility he waited 2 hours and was continuing to vomit and have diarrhoea. The parents feeling frustrated and anxious took him to a nearby provincial hospital. By this time he was lethargic. They rushed him and put him on the Clinical Officer’s couch. They were told the child will be seen after they have paid Kshs 300 for the file. The father rushed to the reception area and paid the money after waiting for other clients to pay. When he came back to where he left the child, he found that he had not yet been seen. After he produced a receipt, Kazungu was seen and admitted to the ward. He recovered after 2 days. |
| 4
a) What do you think of the services provided to this child at?
…………………………………………………………………………………………………………………… ……………………………………………………………………………………………………………………
…………………………………………………………………………………………………………………… …………………………………………………………………………………………………………………… b) Does your facility have a system of sorting out very sick children and having them seen urgently? …………………………………………………………………………………………………………………… …………………………………………………………………………………………………………………… c) If yes, describe the system in place …………………………………………………………………………………………………………………… …………………………………………………………………………………………………………………… d) If no, do you think you can help to implement one? …………………………………………………………………………………………………………………… ……………………………………………………………………………………………………………………
|
This case illustrates the following two points:
- It is important to attend to sick children as soon as possible.
- Sick children should be seen even before registration or paying for services.
Availability of essential drugs and supplies at all times is important. An emergency can happen any time. Therefore it is good to be always prepared.
Let us look at the second case study
| 2
Baby Jane who is 8 months old was brought by the mother to hospital because of fever and vomiting. The waiting area was full of sick children. They waited for 2 hours to be seen. While they were waiting, Jane started convulsing and vomiting. Her mother rushed her to the emergency area screaming. The nurse tried to clear the airway by suction, but the suction machine had been borrowed by another area. So she put the infant on left side, head down and used gauze to clear the mouth. As Jane continued to convulse, she looked for diazepam to give rectally. It was not there as the emergency tray had not been updated that morning. So she asked a support staff to rush to the adult casualty to get some. Someone else had gone to bring the suction machine. By the time Jane was stable, she had been blue for several minutes. In what way could the problems faced by Jane been avoided? …………………………………………………………………………………………………………………… ……………………………………………………………………………………………………………………
|
I am sure from this casestudy you can see that Jane’s baby almost died because the emergency areas was not prepared with all the necessary equipment and supplies. It illustrates the importance of always being prepared in terms of essential equipment, drugs and supplies.
The problems encountered by baby Jane and the staff could have been avoided if staff had been familiar with Emergency Triage Assessment and treatment (ETAT). Let us briefly look at ETAT.
What is Emergency Triage Assessment and Treatment (ETAT).
As I mentioned earlier, ‘Triage’ simply means sorting out. That is, assigning a person to see that very sick children are seen first and emergencies dealt with immediately. ETAT demands that very sick children should not have to be registered first before they are seen. Also newborn babies who are less than 2 months old should be seen quickly, as sometimes they may die quietly in the queue. Anyone can be trained to do triage, even an askari or records clerk. Having staff trained in ETAT helps to also ensure that the essential drugs and equipment are always available in the emergency area. This way, the scenario depicted in Case study 2 can be avoided.
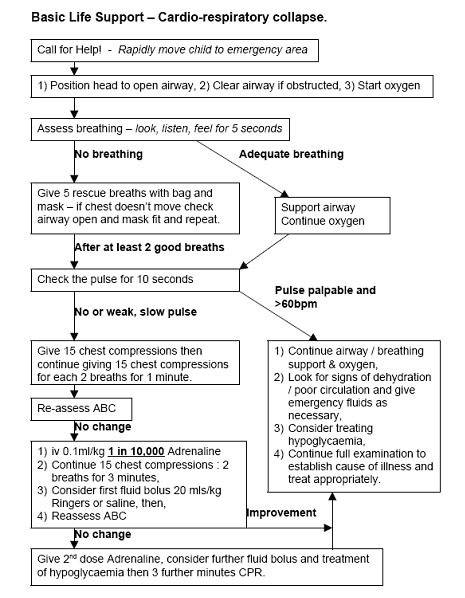
Another important thing to have in emergency areas is wall charts which give staff instructions on what to do. Examples of these wall charts are:
- Charts on resuscitation of children which should be displayed in all emergency areas including wards;
- Newborn resuscitation charts which should be in labour ward, nursery, maternity theatre;
- Fluid management plans;
- Dosages and routes of administration of drugs.
The Kenya Ministry of Health has included all these charts in a booklet titled ‘Basic Paediatric Protocols’. This booklet is available free of charge from the Ministry of Health website.(www.health.go.ke). See figure 2.2 for a sample chart on basic life support. You will also find some of some of these charts in subsequent units of this course where the specific diseases and their management are discussed.
Figure 2.2: Chart on Basic Life Support Chart. Source: MOH, Paediatric Protocols National Policies for Standard Care
In its efforts to improve the health care of sick children in hospitals, our government has developed a number of policies following the IMCI guidelines. The specific policies that should be followed include the following:
- Children should be allowed to stay with a caretaker in the ward;
- All children admissions should be given Vitamin A unless they have received a dose within the last one month. Malnourished children with eye signs should receive repeated doses;
- All newborn admissions aged less than 14 days should get Vitamin K unless it has already been given;
- Newborns should be given Vitamin K and eye prophylaxis at birth;
- Immunizations should be given daily to avoid missed opportunities;
- Missed immunizations should be given before a child is discharged from the ward;
It is Ministry of health policy that under-fives should not pay for health services.
Policies on the Hospital Environment
Within the hospital environment when children are hospitalised, the following aspects of in-patient care are important:
- A child should stay with the mothers or caretaker;
- Breastfed children should get breast milk and breastfeeding should be promoted. This means that babies below 6months of age should be exclusively breastfed. Hospital staff should not give these babies any other food. Have you found 3month old baby being given porridge in the hospital? You should discourage this and encourage the mother to practice exclusive breastfeeding;
- Children should get feeds that are appropriate and commensurate with their age;
- Caretakers should be counselled and educated on their children’s illness;
- As much as possible, admissions should receive diagnostic counselling and testing for HIV. Those children who are eligible for ART should be able to access this service;
- Psychosocial stimulation is important for children recovering from illness. It is therefore important that children’s wards have a designated, safe play area. This is especially so for malnourished children;
As a health worker, you have an important role to play in the implementation of these policies which are crucial in improving the health of children.
3. Improvement of Family and Community Practices
The 3rd component of IMCI addresses the household and community. As you maybe aware most sick children die in the community. Also, most of the causes of ill health can be prevented. If communities and households observed some positive practices, it would go a long way in reducing child deaths. In this component called community IMCI (cIMCI), 16 important practices have been adapted internationally. In addition, Kenya’s Ministry of Health has added 4 more practices. These practices have been grouped into the following 4 broad areas:
A. Growth Promotion and Development
- Exclusive breastfeeding for 6m
- Appropriate complementary feeding from 6m whilst continuing BF up to 24m
- Adequate micronutrients through diet or supplementation
- Promote mental and psychosocial development
B. Disease Prevention
- Proper disposal of faeces, hand washing etc
- Child sleeps under ITN
- Prevention and care of HIV/AIDS
- Prevent child abuse/neglect & taking appropriate action
C. Home Management
- Continue to feed and offer more food & fluids when child sick
- Give child appropriate home treatment for infections.
- Take appropriate actions to prevent and manage child injuries and accidents
D. Care seeking and compliance
- Take child to complete full course of immunization before 1st birthday
- Recognize when child needs treatment outside home and take to HW
- Follow Health Worker’s advice about treatment, Follow Up and referral
- ANC attendance and TT vaccination during pregnancy
- Active participation of men in childcare and reproductive health activities
In addition to the above 16 practices, Kenya has added the following:
- Birth registration and issuance of birth certificate
- Growth monitoring
- Household water safety
- Control of indoor air pollution
In the current National Health Sector Strategic Plan II (2005-2010), the Ministry of Health has stated that health care strategies will start at the community level. The plan has also underlined the important role that will be played by community owned resource persons (CORPS) in the achievement of its objective. In the area of IMCI, CORPS will play a key role in promoting the above practices to improve the health of children and communities. Apart from that, they will be involved in other health aspects as will be decided by the various programs in the Ministry of Health.
Let us consider the importance of the practices in the first 4 broad areas we first listed.
A) Growth Promotion and Development
- Exclusive breastfeeding for 6months
- Appropriate complementary feeding from 6m whilst continuing BF up to 24m
Considering the above 2 practices, it has been shown that exclusive breastfeeding (no food or water except medicine for the first 6 months) protects infants from pneumonia and diarrhea. However many babies in our communities are weaned as early as 2 weeks. The Kenya Demographic and Health Survey 2003 shows only 2.6% of babies are exclusively breastfed at 6 months. As health workers, we should promote breastfeeding. All mothers, unless medically indicated, should breastfeed their babies exclusively for the first 6 months.
Adequate micronutrients through diet or supplementation
One of the important micronutrients which is supplemented is Vitamin A. This is given to children aged between 6 months to 5 years. As most mothers stop taking their children to the clinic after they get the last vaccine (Measles at 9 months), it is important for them to bring their children who are under 5 years s to the clinic for weighing and vitamin A supplementation every 6 months.
B) Disease Prevention Diarrhoea and malaria are the important causes of disease and death. It is therefore important to prevent them. Safe disposal of faecal material and hand washing need to be promoted. Whereas families may have and use pit latrines, sometimes babies’ stools are not disposed off safely as mothers may not think it is an important cause of infection. You need to educate mothers on the need for proper disposal of all waste including the baby’s stool.
To prevent malaria in vulnerable groups ( that is children under 5 years and pregnant women) it is very important to promote the use Insecticide Treated Nets (ITNs). These groups are required to sleep under ITNs every night. Recently the Ministry of health distributed 3.4 million ITNs to pregnant women and under-fives in those districts where malaria is a problem.
The other practice under this group is the prevention and care of HIV infection in children. This is approached by:
- Prevention of HIV infection in the general population. This includes women of child bearing age;
- Prevention of pregnancy in HIV positive women;
- Prevention of mother to child transmission of HIV;
- Care, treatment and support of HIV infected women, children and families;
Prevention of mother to child transmission (PMTCT) of HIV is being carried out in many health facilities. It is important to ensure that all pregnant women have access this service. This will reduce the number of children who get infected with HIV. Almost 60% of admissions in Kenyatta National Hospital have HIV as underlying condition. You will learn more about the management of children with HIV/AIDS in Unit 14.
It is also our responsibility as health workers to prevent child abuse and neglect by taking appropriate action. We have a great role to play in recognising and managing children who are abused or neglected. You should report these incidences to the children’s officers so that they can take the appropriate action.
C) Home Management
The practices under this area include the need to continue feeding and offering fluids to sick children as well as giving sick children the appropriate home treatment for infections. As you are well aware, this is a good principle of home care. Sick children often have a very poor appetite and it is our responsibility as health worker to educate the caretakers to continue feeding the child. You should also counsel them on the danger signs so that they can bring their children back if they get worse. This is especially so in diseases like diarrhoea. This prevents both dehydration and malnutrition. In the case of diarrhoea, there are three rules of home treatment which you should teach them. These are:
- more fluids
- continue feeding
- when to return immediately.
These will be covered in more detail in Unit 11 on diarrhoeal diseases. In addition, the Ministry of health, Division of Child Health has developed guidelines for home management of diarrhoea as well as guidelines for community health workers.
D) Care seeking and compliance
This group of practices emphasise the importance of Immunization of babies and pregnant women. It is the most effective method of preventing diseases like polio, measles and neonatal tetanus. Involving all family members in ensuring that this is done will prevent outbreaks of disease. Early care seeking is crucial in preventing morbidity and mortality
SUMMARY
Well done, you have now come to the end of this unit. We hope you now understand the IMCI concept and its various components. You will see this concept applied in subsequent units when we discuss specific childhood conditions.
PRACTICAL EXERCISE
1. Visit the children’s ward or the MCH clinic in your facility. Talk to 10 mothers with babies aged who are under 6 months and find out the following.
- How many are still on exclusive breastfeeding?
......................................................
- If not on exclusive breastfeeding, what was the earliest age of weaning?
..........,
- What was the latest?
.........................................
- What were the reasons they gave you for starting early weaning?
.........................................
- Write a short summary of the advice that you would you give them?
.........................................
2. Review the national policies we discussed on standard care. List down the ones which have been implemented in your health facility stating how they have been implemented.
.......................................
.......................................
.......................................
.......................................
.......................................
.......................................
Send your answers together with the attached assignment.
|
AMREF DIRECTORATE OF LEARNING SYSTEMS DISTANCE EDUCATION PROGRAMME
Student Name _________________________________________ Address ______________________________________________
Unit 2: Assignment Integrated Management of Childhood Illnesses Answer all the questions given. When you have finished, mail it or bring it in person to AMREF’s Distance Education Courses. Our address is given at the end of this assignment. 1. What are the three components of the IMCI strategy? a) …………………………………………………………………………………………………………………… …………………………………………………………………………………………………………………… b) …………………………………………………………………………………………………………………… …………………………………………………………………………………………………………………… c) …………………………………………………………………………………………………………………… …………………………………………………………………………………………………………………… 3. In IMCI, all children are first assessed for danger signs. What are these danger signs? …………………………………………………………………………………………………………………… …………………………………………………………………………………………………………………… …………………………………………………………………………………………………………………… ……………………………………………………………………………………………………………………
…………………………………………………………………………………………………………………… …………………………………………………………………………………………………………………… …………………………………………………………………………………………………………………… ……………………………………………………………………………………………………………………
…………………………………………………………………………………………………………………… …………………………………………………………………………………………………………………… …………………………………………………………………………………………………………………… ……………………………………………………………………………………………………………………
5. In order to reduce deaths of children in emergency areas of hospitals, name 3 important items which should be displayed in these areas in order to assist health workers manage emergencies appropriately? …………………………………………………………………………………………………………………… …………………………………………………………………………………………………………………… …………………………………………………………………………………………………………………… ……………………………………………………………………………………………………………………
…………………………………………………………………………………………………………………… …………………………………………………………………………………………………………………… …………………………………………………………………………………………………………………… …………………………………………………………………………………………………………………… 7. What are the 3 rules of diarrhoea home management? …………………………………………………………………………………………………………………… …………………………………………………………………………………………………………………… …………………………………………………………………………………………………………………… …………………………………………………………………………………………………………………… 8. Name the 4 practices under growth promotion and development. …………………………………………………………………………………………………………………… …………………………………………………………………………………………………………………… …………………………………………………………………………………………………………………… …………………………………………………………………………………………………………………… 9. What are the 4 family and community practices added by Kenya to make 20 practices? …………………………………………………………………………………………………………………… …………………………………………………………………………………………………………………… …………………………………………………………………………………………………………………… ……………………………………………………………………………………………………………………
|