Lesson 14: HIV/AIDS
Contents
INTRODUCTION
In the early 1980s a new pandemic emerged. There is now no country that is not reporting cases. Majority (over 60%) of cases are in sub-Saharan Africa. About 10% of these are children. In fact about 90% of paediatric HIV/AIDS are African children. Worldwide HIV/AIDS is responsible for about 3-7% of deaths in children under 5 years of age. In Africa the deaths are most probably higher compared to the world in general. Advances in diagnosis and care and treatment have increased survival of both adults and children. Since HIV infection is incurable the stress now should be on prevention.
In Kenya the first case was reported in 1984. Since then the prevalence has escalated to involve the whole country. Originally the infection was more prevalent in urban areas but is now found in rural areas as well. Some parts of the country are more affected than others. Reported figures change from year to year so it is important to keep abreast.
|
By the end of this unit you should be able to:
|
14.1 What is HIV/AIDS
Begin by doing this activity
| 1
What do the letters HIV and AIDS stand for? Human Immunodeficiency Virus and Acquired Immunodeficiency Sydrome _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
|
Now read through the text below and see if your ideas are included.
HIV - Human Immune deficiency Virus AIDS – Acquired Immune Deficiency Syndrome
In adults, HIV infection remains in the body for a long time. The person infected is healthy in all respects. When the immune cells in the body have been reduced the infected person starts getting serious and recurrent infections. This is when the infected person is said to have AIDS.
In children however, HIV infection in children occurs in the context of an immature immune system resulting in more frequent and severe common infections and an increase in opportunistic infections. Although HIV infected infants are generally asymptomatic at birth, most of them develop severe symptoms in the first two years of life and die.The course varies and is thus divided into two – the rapid progressors who often die within two years and the slow progressors whose course may behave like that of adults.
| 2
What are the key differences in chronic HIV care between adults and children? _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
|
Now read through the following text and see if your ideas are included.
The key differences in chronic HIV care between adults and children are as follows:
- Young children have immature immune systems and thus are susceptible to common infections as well as opportunistic infections.
- Due to maternally acquired antibodies, a positive rapid HIV test is not definitive of HIV infection in HIV-exposed children below 18 months. However, a negative test is useful because it excludes infection acquired from the mother.
- Normal CD4 counts are higher in young children than in adults and decrease with age to reach adult levels around the age of 6 years.
- ARV drugs are handled differently in children's bodies, affecting the doses that are needed. Dosages in children need to be adjusted according to weight as the child continues to grow.
- Counselling children for disclosure of their HIV status, to discuss ART, and to support adherence to ART requires special skills in communication.
14.2 MODES OF TRANSMISSION
Now let us look at how a child acquires the infection
Start by the following activity
| 3
What are the modes of transmission in children? _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ Are all babies born to HIV infected women also infected? _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ What is the estimated risk of transmission? _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ Should HIV infected mothers breastfeed? _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
|
Compare your response to what is given.
HIV spreads to children in four ways.
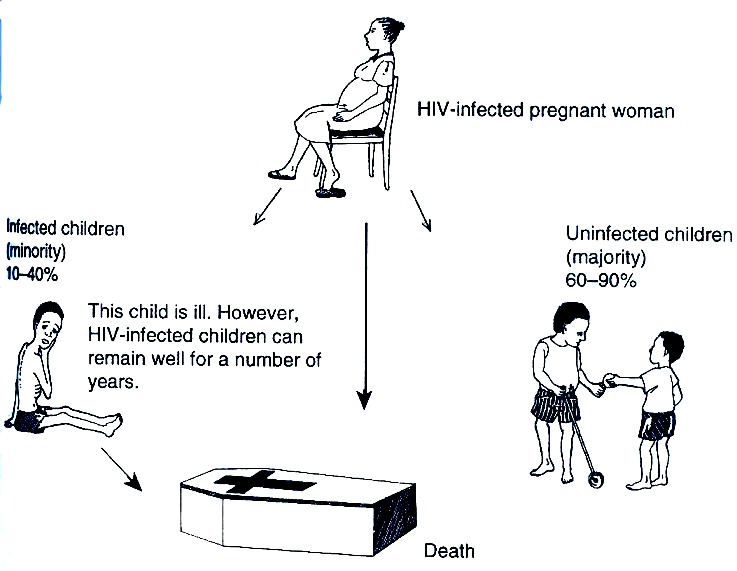
- Vertical transmission also known as mother to child transmission (MTCT). This may occur during pregnancy, during delivery or through breastfeeding. Most infected children receive the virus through this way. Indeed, if a pregnant mother is infected, the chance of her child being born infected is approximately 1 in 3). However, most infected mothers will not infect their infants, although the probability of infection is higher if the mother is sick with AIDS. Vertical transmission can be reduced by quality obstetric care, use of ARV during pregnancy, perinatally to the mother and postnatally to the baby, as well as counselling on feeding options.
Figure 14.1: Vertical transmission of HIV infection
- Blood transfusion. Over 95% of children who get blood from an infected person will get HIV;
- Sexual intercourse. Although this is the main mode of transmission among adults, these days with increasing cases of rape and defilement, young children are getting infected through this way. Teenagers are also at vulnerable as they may be coerced to have sex or experiment with early sexual intercourse.
- Contaminated needles. HIV infection may be spread through poor standards in our health facilties, such as reuse of syringes and needles without adequate sterilisation. Infection can also be spread through skin cutting by untrained persons, illicit injections, scarification and circumcision.
14.3 SIGNS AND SYMPTOMS
Begin by doing this activity.
| 4
Write down all signs that may indicate that a child has HIV infection _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
|
Compare your answer to the following:
There are no specific features but HIV infection is suspected when a child has any of the following:
- Chronic Otitis media
- Persistent parotid enlargement
- Slow growth or weight loss that fails to respond to adequate nutrition
- Recurrent serious infections e.g. pneumonia
- Tuberculosis
- Recurrent and persisted diarrhoea
- Oral thrush beyond the neonatal period often difficult to treat and recurrent, oro-pharyngeal candidiasis
- Various skin eruptions
- Herpes zoster
- Neurological dysfunction either delayed or regressed milestones
- Failure to thrive
Remember that many of these problems are common in children who may not necessarily have any HIV infection. Howeevr, you should have a high index of suspicion so that you do not fail to detect the infected child. Growth failure may be a good indicator. So as you monitor growth in the MCH watch out for those children who fail to respond to adequate nutrition counselling.
The HIV adapted IMCI Guidelines ( See Table 14.1) are also very useful in helping you to identify likely symptomatic cases in children below 5 years.
As we mentioned in Unit 3, the case management process of IMCI shows you the sequence of steps to follow and provides you with information on what to do at each step. The charts describe the following steps:
- Assess the sick child - taking a history and doing a physical examination
- Classify the illness - making a decision on the severity of the illness
- Identify treatment
- Treat the child - giving treatment in the clinic, prescribing drugs or other treatments to be given at home and also teaching the mother how to carry out the treatments
- Counsel the mother- includes assessing how the child is fed and telling her about the foods and fruits to give the child and when to bring the child back to the clinic
- Arrange follow up care
As you can see from Table 14.1, classifications is not based on the diagnosis of a specific disease. Instead, they are categories that are used to determine treatment. When using this process, selecting a classification from the chart is sufficient to allow you to “identify treatment” for a child.
A two-step process is used to identify likely symptomatic cases:
- An initial screening for four conditions (using IMCI classifications) and
- A more complete assessment if any one of the four conditions is present. If on assessment, two conditions are present, the child is classified as symptomatic HIV.
- Pneumonia
- Persistent diarrhoea now or by history
- Ear discharge (acute or chronic)
- Very low weight for age.
Less than three of the above features is classified as No suspected symptomatic HIV infection.
Always determine the HIV status of a sick child as follows:
Table 14.1: Determining HIV Status of a child.
| ASK: |
|---|
|
|
LOOK AND FEEL:
|
|
| Positive HIV antibody test in child > 18 months of age | HIV INFECTION* |
|
| Mother positive (child not tested, and < 18 months)
OR Child < 18 months tested and found to be antibody positive Two or more HIV-related conditions:
|
POSSIBLE SYMPTOMATIC HIV INFECTION in an exposed child |
|
- A known HIV case without symptoms should be managed in a similar way.
14.4 DIAGNOSIS OF HIV INFECTION IN CHILDREN
Begin by doing this activity
| 5
Can an antibody test (Eliza or rapid test) detect all infected children from birth onwards? _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
_____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
_____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
|
Compare your answer with the following
Antibody test:
A baby will carry antibodies passed on from the mother during pregnancy. So all babies born to HIV infected mothers will have a positive test whether they are infected or not. If the baby is not infected these antibodies will gradually reduce and disappear by 12-18 months. If the test is positive beyond 18 months then the child is infected.
Antigen test (test for presence of virus)
For children less than 18 months HIV infection can only be confirmed by tests that detect the virus or an antigen test, for example, PCR or viral culture. The PCR test can be done using a dry blood spot (DBS) sample. These tests are expensive and are usually not available in most facilities. However you should try tobe familiar with the services available in the region where you work in and where a regional laboratory is that can conduct an antigen test is located.
CD4 cell count:
The virus infects and replicates in a type of lymphocyte referred as a CD4 lymphocyte. As the infection progresses, many of these cells are destroyed and the body cannot replace them at a fast rate. When this happens, then the count drops gradually. This drop in CD4 cell count is used to detect the degree of immunological suppression. Absolute CD4 cell count varies with the age of the child so in children less than 6 years the cell percentage which is constant is used instead.
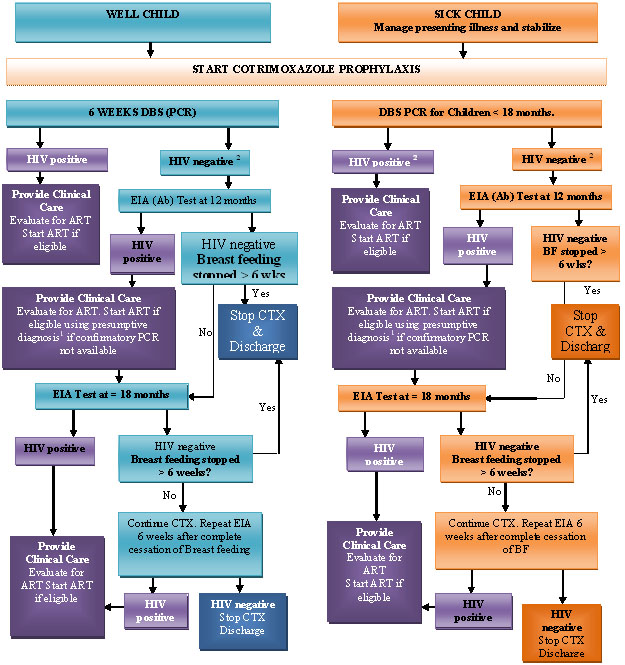
Figure 14.1 below illustrates how to diagnose HIV infection in infants exposed to HIV in the mother. A negative HIV antibody test will rule out maternally acquired infection in a child who has stopped breastfeeding.
Thus there are three groups of children born to HIV-infected women:
Group 1: children with negative antibody tests; Group 2: children with positive antibody tests but who are not HIV-infected; Group 3: children with a positive antibody test and are HIV-infected.
All the 3 groups of children have been exposed to HIV infection during pregnancy. Remember, exposure to HIV infection will continue as long as these children breastfeed. That is why it is very important for you to confirm HIV exposure in children attending the child welfare clinic.
You can confirm HIV exposure by:
- Asking the mother if she knows her HIV status or if she is receiving HIV care;
- Checking the mother’s antenatal card for an indication of her HIV status (a test is done during ANC);
- Advising the mother for the need to test the child. If the mother is willing she can be tested and if her test is positive there is no need to test the child.
HIV-exposed infants as well as children who are confirmed to be HIV-infected will need chronic HIV care including antiretroviral therapy (ART). That is why it important for you to determine whether or not an infant has been exposed to HIV as early as possible, when they come for routine immunization, MCH or other in-patient services. Once it is confirmed that an infant has been exposed to HIV, confirmatory diagnosis using PCR where accessible should be done as per the diagram below. The acute care of sick HIV-infected children is addressed by the IMCI guidelines which we discussed in Unit 2 of this course. Table 14.1 summarises the diagnosis of HIV infection.
Table 14.1: Summary of Laboratory Diagnosis of HIV in Children.
(Source:Primary level training for comprehensive management of HIV)
| Age | HIV diagnosis is confirmed as follows: |
|---|---|
| Children over 18 months | Positive HIV antibody tests (rapid or long EIA) |
| Children under 18 months | Positive HIV PCR from age 6-8 weeks or as soon after, during routine child welfare clinic visits |
| Children under 18 months where PCR is not available | Positive antibody test after the child is > 18 months |
Remember! In addition to using the IMCI guidelines, you should still carry out diagnostic testing in all sick children. This is in order to avoid missed opportunities. If a child is below 18 months of age you should determine their exposure status if you find them to be exposed to HIV, you should have a DNA PCR done or refer to a facility where it can be done.
|
|
14.5 STAGING
| 6
What is HIV staging? _____________________________________________________________ _____________________________________________________________ _____________________________________________________________ _____________________________________________________________ _____________________________________________________________ _____________________________________________________________
|
Now confirm your answers as you read the following discussion.
HIV disease in children may manifest in two ways:
- Conditions unusual in HIV negative children such as Pneumocystis pneumonia (a kind of severe HIV-related pneumonia)
- Non-specific conditions such as severe malnutrition, swollen glands, enlarged liver or spleen
- Common bacterial infections also commonly seen in HIV negative children. .
In resource-poor communities where medical facilities are poorly equipped, it is not possible to use CD4 and viral load test results to determine the right time to begin treatment. That is why the World Health Organization (WHO) developed a staging system for HIV disease based on clinical symptoms.
Staging is done by using the clinical signs as well as immunologically.
Clinical Staging
The WHO clinical staging helps you to estimate the degree of immune deficiency that a child has. WHO clinical staging should only be carried out in patients who have a confirmed HIV diagnosis. Children under 13 years are staged differently while adolescents are staged as adults.
A stage 1 and 2 clinical status indicates that the immune system is not yet seriously affected. Stage 3 and 4 indicates advanced immune deficiency.
The last row in each table indicates when ART is given. Before ART can be started you must have a confirmed diagnosis of HIV infection, except in children with presumed severe HIV infection.
Presumed severe HIV infection is a diagnosis made in a child under 18 months when confirmation is not possible with PCR test. The child has to be known to be HIV-exposed (antibody positive in child or in mother) and must have severe clinical illness or be symptomatic with 2 or more of the following:
- Oral candidiasis (thrush)
- Severe pneumonia requiring oxygen
- Severe wasting/malnutrition
- Severe sepsis requiring injectable antibiotics
- Other factors that support the diagnosis of severe HIV infection in an HIV sero-positive infant are recent maternal death or advanced HIV disease in mother.
The four stages can be summarised as follows:
- Stage 1: is the asymptomatic or mildly symptomatic stage;
- Stage 2: is when the child starts having skin lesions, oral lesions, ear infections, and parotid enlargement.
- Stage 3: is when serious features appear - these include severe and recurrent pneumonia, Tb, and persistent diarrhoea;
- Stage 4: severe wasting, disseminated Tb, and many complications some of which are only found in HIV infected patients e.g. pneumocystis jiroveci (PCP) pneumonia, severe CNS and other organ involvement.
See Tables 14.2 for the WHO paediatric staging of HIV and AIDS.
Table 14.2 : WHO paediatric staging of HIV and AIDS disease (any one condition in the highest staging is adequate)
| WHO Paediatric Clinical
Stage 1 Asymptomatic |
WHO Paediatric Clinical
Stage 2 Mild Disease | |
|---|---|---|
| Growth | ||
| Symptoms/
signs |
No symptoms or only:
|
|
| ARV
Therapy |
Indicated only if CD4 is available:
< 18 months &CD4 < 25% (<1500) 18 mo -5 yrs &CD4 < 15% (<500 ) > 5 yrs & CD4<10% (<200 ) |
Indicated only if CD4 or TLC is available:
Same as stage I OR < 18 months &TLC<4000 cells/mm3 18 mo-5 yrs & TLC<2500 cells/mm3 > 5 yrs and TLC<2000 cells/mm3 |
| WHO Paediatric Clinical
Stage 3 Moderate Disease |
WHO Paediatric Clinical
Stage 4 Severe Disease (AIDS) |
|---|---|
|
|
|
|
| Start ART:
All children irrespective of CD4 or TLC; |
Start ART irrespective of CD4 count Start ART in presumptive severe HIV infection in children < 18 mo where PCR is not available |
For staging cases clinically, most of the clinical conditions used for clinical staging for adults are generally similar for children (for example, Kaposi’s sarcoma or oesophageal thrush). Persistent diarrhoea is defined as persistent or recurrent diarrhoea lasting more than 14 days (this is the same definition as in IMCI ).
Other conditions specific to children are defined below.
Severe Malnutrition—is defined as either visible wasting or weight for age
- Generalized persistent lymphadenopathy—development of persistent, lymphadenopathy in early infancy, consisting of enlarged lymph nodes (>0.5 cm) in two or more regions other than the inguinal area without any apparent underlying cause.
- Parotid enlargement—chronic parotid enlargement is defined as one-sided or bilateral parotid swelling (just in front of the ear) with or without pain and fever and persisting for more than 2 weeks. Consider mumps, secondary infection if painful parotid glands in febrile patient
- Encephalopathy—Failure to attain or loss of developmental milestones or loss of intellectual ability; impaired brain growth or acquired microcephaly
- Lymphoid interstitial pneumonia (LIP)—Slowly progressive interstitial lung disease with bilateral reticulonodular interstitial pulmonary infiltrates present on chest X-ray for > 2 months with no pathogen identified and no response to antibiotic treatment. Occurs among children more than 2 years old. Consider TB and rule out history of TB in a member of the immediate family.
- Pneumocystitis pneumonia—Severe pneumonia with cyanosis in a child less than one year old or dyspnoea on exertion or non-productive cough of recent onset in older children with chest X-ray evidence of diffuse bilateral interstitial infiltrates and no evidence of a bacterial pneumonia.
Immunological staging
Immunological staging takes into account the number or percentage of CD4 cells. There are 3 stages here ranging from no to severe immune suppression.
14.6 TREATMENT AND MANAGEMENT
A lot of advances have occurred in the treatment and management of HIV to the extent that people infected with the virus can now survive for a long time. So when a diagnosis is made the child should be referred to a centre where effective care can be done. We can divide this care into 4 or 5 components.
1. Prevention:
- Ensure that the child is immunised according to the national guidelines; The only exception is the BCG immunization which should not be given to severely sick children (WHO stages 3 or 4).
- Give prophylaxis against PCP using daily doses of cotrimoxazole. Cotrimoxazole prophylaxis should be offered to:
- HIV-exposed children
- HIV-infected children
HIV-exposed children
According to the National ART Guidelines (2005) section 5.1, in all HIV-exposed children, you should start cotrimoxazole at 6 wks or when first seen.
A child is said to be exposed to HIV infection if any of the following circumstances prevail:
- If they are born to a woman confirmed to be HIV-positive, are < 18 months of age and they have not had a PCR test done;
- If the child is under 18 months of age and has a positive HIV antibody test and they have not had a PCR test ;
- If the child is breastfeeding at any age and their mother is confirmed to be HIV positive.
HIV-infected child
Start Cotrimoxaole routinely in all HIV-infected children regardless of age, immune status or treatment status. Cotrimoxazole syrup is administered once daily. If syrup is unavailable, paediatric tablets may be used or adult tablets can be split appropriately as shown below. In order to ensure continuous access to medication, you can switch from syrup to tablets. Table 14.4 below gives the dosages for contrimoxazole.
Table 14.4. Cotrimoxazole (trimethoprim-sulfamethoxazole or TMP/SMX) dosages
| Weight of child (Kg) | 240 mg per 5 ml Suspension | Single Strength (SS) Tablets 480 mg | Double Strength (DS) Tablets 20mg/100mg |
|---|---|---|---|
| 1-4 | 2.5 ml | ¼ tablet | |
| 5-8 | 5 ml | ½ tablet | ¼ tablet |
| 9-16 | 10 ml | 1 tablet | ½ tablet |
| 17-30 | 15 ml | 2 tablets | 1 tablet |
| >30 | 20 ml | 2 tablets | 2 tablets |
Cotrimoxazole prophylaxis should be continued indefinitely.
Side effects of cotrimoxazole are the same in children and adults. See section 7.2 of the Primary-level Handbook. Children who cannot tolerate cotrimoxazole should be referred to a senior clinician for management
- Prevent tuberculosis (Tb) by identifying young children whose parents have Tb and putting them on prophylaxis if necessary. Children exposed to “open TB” (or whose close contacts have sputum positive TB) should be assessed for TB and if found to be well given INH to prevent TB. A clinician should make the decision on whether or not a child exposed to open TB should get Isoniazid Preventive Therapy ( IPT).
- Encourage and reinforce the use of insecticide treated nets.
2. Nutrition Counselling:
All HIV-infected children should have a nutritional assessment during each clinical visit. The growth chart should be used for younger children to ensure that the child continues to grow as desired. Food for treatment should be provided for malnourished children and nutritional supplement (food) given to those children who are underweight. All HIV infected children should be given multivitamin supplements since many patients have diets deficient in micronutrients. This can delay disease progression. Nutritional needs of an HIV infected child is higher than in a non-infected one. When they are sick their appetite is poor. Teach parents or caregivers to make food attractive and nutritious.
3. Treatment of opportunistic infections such as Tb, PCP, candidiasis.
You should treat opportunistic infections in children before starting ART. Table 14.5 below gives you the guidelines on treatment of opportunistic infections.
Table 14.5: Guidelines on the treatment of opportunistic infections
| If child has this opportunistic infection or other clinical problem: | Follow these instructions
(use IMCI guidelines): |
|---|---|
| Severe illness or any severe classification in IMCI
(e.g. severe pneumonia) |
Stabilize the child and then refer to hospital for treatment and to decide ARV regimen. Follow treatment plan when child returns. |
| Non-severe pneumonia | Treat as in IMCI or national guidelines.
(Malaria, UTI, sore throat). Do not start ART until treatment completed and no longer febrile. Refer if persistent fever. |
| Other acute infections
(malaria, UTI, sore throat) |
Treat with antibiotics/ anti-malarials, use amoxicillin especially if child on cotrimoxazole. Wait for two weeks (to be sure this was not TB) before starting ART. If no improvement, Refer. |
| Drug reactions | Do not start ART during an acute reaction. If already on ART, section 8.12 of the Primary-level Handbook) |
| Prurigo or other known
chronic skin problems |
Do not delay ARV therapy. Manage chronic skin problems. |
| Oesophageal thrush and
able to swallow fluconazole syrup or capsules |
Start ART after fluconazole treatment if able to swallow. If not able to swallow, refer. |
| Persistent diarrhoea | Put on nutritional management and re-hydrate (use IMCI guidelines). Do not delay ART waiting for resolution. |
| Anaemia | Refer if severe anaemia.
Start treatment for non-severe anaemia (use IMCI guidelines). Do not delay ART. |
| Persistent fever without explanation | Stabilise the child. Give antipyretics. Consult a clinician. |
Treat tuberculosis before initiating ART
Tb diagnosis in children is a particular challenge because sputum collection from young children is difficult. You should refer any child with fever, weight loss or failure to gain weight despite corrective measures to a clinician for review for TB.. Many children with HIV have Tb.
Before we proceed with this discussion do the following activity.
| 7
List the signs and symptoms that occur in HIV and Tb _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
|
Compare your response to the following:
- Failure to thrive or weight loss
- Chronic cough
- Enlarged lymph nodes
- Persistent fever
It is important that a diagnosis and treatment of Tb is done. If Tb is suspected investigate and refer appropriately to a Tb centre for treatment. In the case that the child requires ARVs, Tb treatment should be started first and then after the intensive phase, ARVs should be given. But if the child is severely immune suppressed, one may not wait for the completion of intensive Tb treatment phase. Such a child should be referred to experienced clinician for appropriate decisions.
4. Antiretroviral Therapy (ARTs).
The decision to start on ART should only be made in consultation with a clinician because of the need for expertise to decide on the clinical staging and sometimes to interpret the lab results. There is also limited experience in the use of these drugs in children.
ARTs are indicated as follows:
- Clinical stage 3 or 4 start ART irrespective of immunological stage
- Clinical stage 3 or 4 with immunological stage 2 or 3
- Immunological stage 3 irrespective of clinical stage.
Before starting ART, you need to consider the following:
- medical eligibility;
- psychosocial eligibility criteria.
Medical eligibility
A clinician should initiate ART in children based on the clinical staging and CD4 count if available. These two factors make up the medical eligibility criteria. In the absence of the CD4 test the following clinical staging table indicates when the child is medically eligible for ART.
Table 14.6: CLINICAL CRITERIA FOR INITIATING ART (In infants and children <14 years)
| WHO Stage | Therapeutic step |
|---|---|
| Stage 4 | Start ART regardless of CD4 |
| Stage 3 | Start ART regardless of CD4 |
| Stage 1 and 2 (require CD4 count) | <18 months: CD4 <25% or <1500
18 months - 5 years: CD4 <15% or <500 ≥5 years: CD4 ,15% or <200 |
| Presumptive Severe HIV disease | Start ART. Confirm HIV diagnosis as soon as possible |
Psychosocial Criteria The psychosocial criteria for initiation of ART includes the following:
- An identifiable parent or guardian who is;
- Able to understand treatment requirements
- Consistently and correctly administer the child’s medication
- Able to attend the HIV clinic appointment regularly
- Sustainable long-term access to antiretroviral drugs.
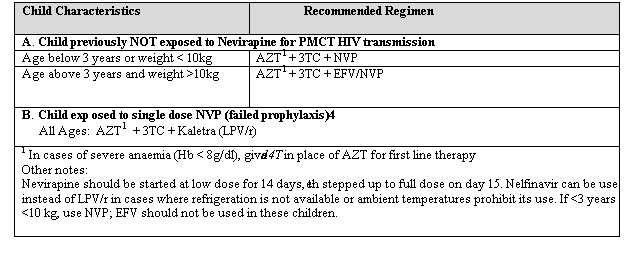
First-line ARV Regimens for Children
There may be several antiretroviral (ARV) drugs available in your health facility in a first-line ARV regimen, such as:
- nevirapine (NVP)
- stavudine (d4T)
- lamivudine (3TC)
- efavirenz (EFV)
- zidovudine (AZT)
Table 14.7. gives the 1st line ARV regimens for children
ARV drug preparations for children
Many ARV drugs are now available in liquid formulations. However, they are often more expensive than adult formulations. Also their storage can be challenging because of large volumes and also because some may require refrigeration. Some liquid formulations also taste bad, which can make them difficult to take.
It is important to pay attention to the shelf life of all ARV drug preparations including liquid antiretroviral preparations.
Some tablets and capsules come in low enough doses to enable accurate dosing for children of most ages (e.g., d4T capsules come in 15, 20, and 30 mg strength, and NFV (nelfinavir) has scored tablets that can be halved). Fixed dose combination tablets suitable for children are becoming more available. These may allow better adherence because of low pill burden.
Well, they present various problems related to the need to cut them up. These are
- Under-dosing of drugs is possible, which can lead to increased risk of resistance;
- Over-dosing of drugs is possible, which can lead to increased risk of toxicity;
- The doses cannot be easily adjusted as the child grows; and
- Some drug combination tablets (e.g., fixed dose AZT/ 3TC) do not have the AZT and 3TC components evenly distributed through the tablet and therefore cutting them could result in wrong dose of either component.
- Adult fixed dose combinations may not contain the appropriate doses of each of the component drugs for children on a weight basis. This is a specific problem for the NVP component of the fixed-dose combination of d4T/3TC/NVP, for which additional NVP may be necessary if tablets are used to treat younger children.
As a health worker it is very important for you to be aware of these problems and to advice the caregiver appropriately.
How do we determine the paediatric drug dose?
Ideally the paediatric drug dose should be calculated per kilogram body weight. You should remember to increase the drug dose as the child grows; otherwise there is a risk of under dosage and development of resistance. Children’s ARV doses are also calculated according to child’s surface area. .
Monitoring Response to ARV therapy
Once a child has been put on ARV they need to be monitored using a certain criteria. This is:
- Clinical
- Laboratory
- Adherence
- Psychosocial
Let us briefly look clinical and laboratory monitoring..
Clinical Monitoring:
At each visit clinical monitoring in children should include:
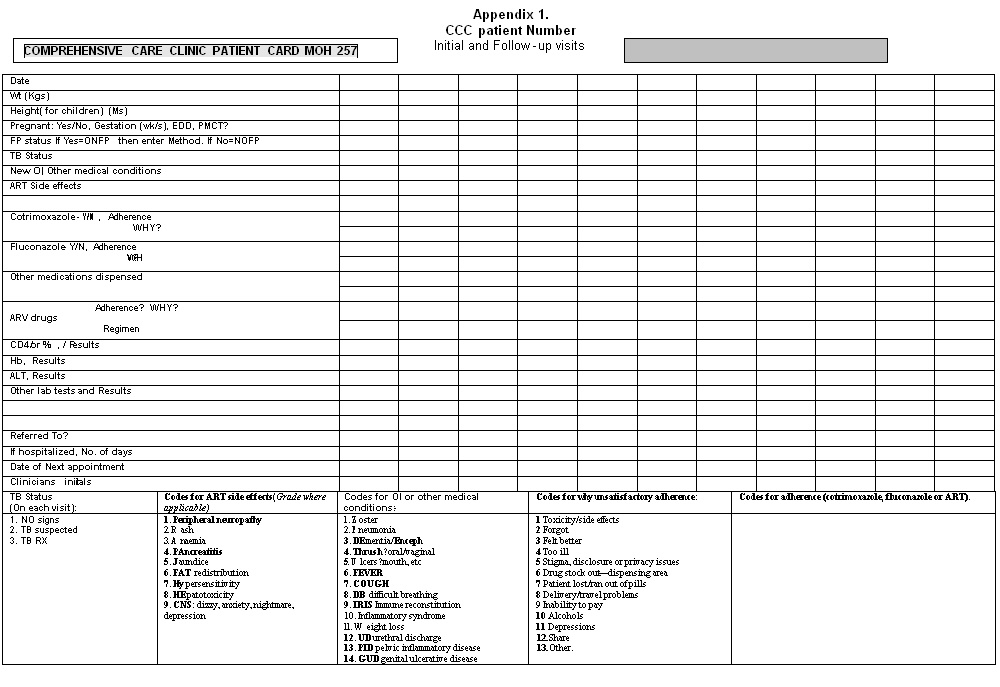
- Measuring of weight and height gain, using growth charts and assessment of developmental milestones. The weight and height should be recorded in the CCC card
- Assessment for symptoms and signs of adverse drug reactions
- Types and frequency of opportunistic infections. Any new OI should be recorded in card
A child’s response to ART is often obvious and clearly seen in a rise in weight, height and wellbeing. Children who fail to gain weight should be assessed for presence of OIs, poor adherence to ART or, failure of ART or poor nutritional intake.
Important Clinical Signs of Antiretroviral Drug Failure
These include:
- Lack of growth response to treatment or
- Falling off the growth curve in children who show an initial growth response to therapy
- Loss of neuro-developmental milestones (regression)
- Recurrent oral thrush and other opportunistic infections.
Continue cotrimoxazole prophylaxis and nutritional supplements (such as multivitamins and protein rich porridge flour). Consult a clinician when addressing on going medical problems and treating infections.
Manage side effects and new symptoms
Children tolerate ART better than adults and experience side effects less commonly than adults. The specific side effects are similar to those seen in adults. Assessment of side effects may be more difficult than in adults because children may not articulate their symptoms. Young children may not complain of headache but they may become irritable to the pain and manifest reduced feeding and reduced activity. Similarly children may not be able to locate pain on the abdomen or neuritis. It is therefore important for you to talk to the caregiver and find out what they think as well as examine the child clinically at every clinic visit.
Laboratory Monitoring
Laboratory tests are used to monitor the body’s response to treatment. Laboratory tests are also used to monitor toxicity that may result from ART.
For treatment response:
- Routine CD4 count or percentage should be done where possible at baseline and every 6 months.
- Viral load measurements, if available, provide a very good indicator of efficacy of ART. Where possible it should be measured at baseline and every 6 months
For monitoring toxicity, tests done should depend on the regimen a patient is on. Absence of laboratory tests should not be a barrier to ART and clinical monitoring of patients. The result of all tests should be recorded in the CCC card (See Annex 1). The card should be used as a tool to monitor the patient’s progress over time (trends).
In addition, we need to monitor the child’s nutritional management, provide psychosocial support, have good communication with the child and disclose the illness in the right way.
Nutritional management: The incidence and severity of opportunistic infections such as tuberculosis and diarrhoea, is not only determined by the nutritional status, but also, these diseases have severe nutritional consequences as they cause appetite loss, weight loss and wasting. Other clinical situations that may impair the nutrition of HIV infected children are: recurrent or chronic infection, fever, intestinal infections, oral or oesophageal thrush and persistent diarrhoea.
The management includes the following:
- Increase energy intakes by 50% to 100% over normal requirements in children experiencing weight loss. In other words a child recovering from illness requires up to 2 times the amount of food they normally would take, this is best given in several small amounts.
- Identify the local foods that are available and affordable to advise the caregiver on energy requirements. For the type of local foods, refer to the local food adaptation table, for example, that of IMCI.
- HIV-infected 6-59 months old children should receive vitamin A supplements(100,000 IU for infants up to 12 months, 200,000 IU for children above 12 months) every 4-6 months. This level is consistent with the current WHO recommendations for the prevention of vitamin A deficiency in all children.
- For persistent diarrhoea, refer to IMCI guidelines
- Feeding and increased fluids should continue during illness. The child may develop nausea and vomiting as a result of ARV drugs. Encourage small frequent fluids and give food that the child likes. Let the child eat before medication. In the child with sores in the mouth, give soft and mashed food or give paracetamol half an hour before solid feeds.
Psychosocial support: HIV in children can be very stressful, and coping with this and other issues in the family, such as illness and loss of parents, shaky economic situations, school, issues surrounding disclosure may be too much for children. As much as possible the child should be assessed for psychosocial problems and attempts made to address these within the community and using all available support groups and agencies. Where necessary, children with serious psychological problems should be referred.
Health facility-based and home-based stimulation of children improve their mental, social and emotional development. Children need care through talking, playing and providing a stimulating environment through providing pictures, sketches, toys, colourful paintings where available. Schedule children’s appointments together with their mothers where applicable. Furthermore, children need to be provided with psychological and emotional support within their family or through other caregivers, and to be able to communicate openly about their own or their family member’s condition so as to give relief to deep fears that are difficult to share.
Good communication with children: When communicating with a child, it is useful to be at the same level as he or she is, for example, sitting or lying on the floor. Children are always suspicious of strangers, try to talk to the child, greet the child, touch the child, stimulate the child with a pen, torch light, paper. A child who has been traumatised by any situation may find it difficult to trust others and particularly adults. In order to win a child's trust, adults require patience and must be consistent in their dealings with the child. The child's feelings must be acknowledged as her/his right.
Children speak three "languages"—the language of the body, the language of play, and spoken language. They often tell their story through their play, their behaviour, and their body language. Through observing the different "languages" of children and how children express their meaning, you can learn about what has happened to the child.
Disclosure to a child: Disclosing HIV status to a child is a process. This should be done in a manner that the child understands and it should be done at a pace that the child can cope with. The prime responsibility for disclosing lies with the parent or guardian and you should be guided by the caregiver and be prepared to give support to the caregiver in this process. It is important to consider the age of the child or the ability of the child to understand and cope with this information. Take time to get to know the child. Use games, objects, activities etc to understand the child.
Before you read on, do the following activity. It should take you 5 minutes to complete.
| 8
What is adherence counselling? Write down your definition in the space below. _____________________________________________________________ _____________________________________________________________ _____________________________________________________________ _____________________________________________________________ ____________________________________________________________
|
Now compare what you wrote down with the information presented in the following discussion.
Adherence Counselling
Adherence is the cornerstone of successful ART in children. Adherence greater than 95% is needed to prevent emergence of drug resistance and ensure long term suppression of viral load. That is why adherence counselling is very vital. ARV treatment is life long and the virus rapidly develops resistance to the drugs if there is irregular dosing. For this reason, starting ARVs should never be done as an emergency. The caregiver is central to the wellbeing of the child. You should therefore prepare them well, and if the child is old and mature enough to understand, they too should be actively involved in discussions on adherence and the adherence preparation process.
If a child misses doses the health worker should find out the reasons why and support the caregiver and the older child in addressing the reason. There are a number of way in which you can support adherence in children. This is by:
- Ensuring a stable environment for the child in the home and constant support of caregiver;
- Preparing the child depending on age and maturity and caregiver well before treatment
- Involving school nurses or orphanage staff, where applicable;
- Selecting appropriate drug formulations, considering factors such as taste and pill burden;
- Demonstrating how the drugs should be taken and asking the caregiver or the older child to demonstrate how they take the drugs;
- Seeing parents and children together to avoid multiple appointments for the parents.
5. Dealing with Stigma:
This is very important during care of all HIV infected persons. Dispelling stigma starts with you! All health workers should dispel the fear in themselves first before they can help clients to live positively with HIV.
|
Dispelling HIV stigma starts with you! Before you can help a client live positively with HIV, you must first dispel the fear in you.
|
Management of Chronic Problems
14.7 PREVENTION OF HIV INFECTION
Start by doing this activity
| 9
List ways you can use to prevent children being infected _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ How you can implement a prevention programme in your community. _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ Is there a value of universal testing? _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
|
Compare you answer to the following:
- Prevention of infection:
Helping people to change behaviour and avoiding cultural practices that may increase the spread of the disease. Using clean/sterile instruments in and out of health care setting.
- Blood transfusion:
Ensure that all blood donors are screened for risky behaviour and all blood used for transfusion is screened for HIV. Remember that the screen is for antibody so a newly infected person can pass undetected. You should also avoid unnecessary transfusions.
- Post exposure prophylaxis:
For rape and defilement cases you should give ARV therapy. All children who are defiled or raped should get ARV within 24-72 hours. Parents need to be educated on this fact so that they bring the child to a health facility as soon as possible. Every health care provider should be up to date with the current ARVs that are recommended for this purpose.
- Preventing Mother to Child Transmission (PMTCT)
This involves taking measures to prevent transmission during pregnancy and delivery, and also counselling on feeding options. The following factors increase the risk of MTCT:
- High viral load – either early in infection or late when features of AIDS appear;
- Severe immune suppression (low CD4);
- Poor obstetrics care leading to trauma to the genitalia or baby, prolonged rupture of membranes(>4hrs) and/or labour;
- Prematurity;
- Breast disease such as mastitis or nipple infections.
Activities of PMCT Programmes
PMTCT programmes have been introduced to all districts and they should be to carry out all the following activities:
Antenatal care:
During antenatal care, you should educate all clients about HIV and encourage testing. Ensure adequate maternal nutrition for all mothers. For those uninfected counsel them on how to remain uninfected. For those who are infected offer either full ART or perinatal ART depending on the mother’s disease stage. Counsel on feeding option and allow parents to choose.
During labour and delivery:
Give ARV (nevirapine) at onset of labour unless mother was already on ARVs. Avoid trauma to the mother’s birth canal and the baby. Avoid artificial rupture of membranes and episiotomy. Give ARV to the baby within 72hrs according to national guidelines.
Post delivery:
By now you should have discussed all the feeding options. There are two options - either breastfeeding or replacement feeding (avoidance of breastmilk). WHO recommends that when replacement feeding is acceptable, feasible, affordable, sustainable, and safe (AFASS) then mothers should avoid breastfeeding. If not then mothers should be counselled on how to safely breastfeed. Recent studies from Africa indicate that replacement feeding is associated with increased morbidity and mortality even when formula is provided by the government. Therefore it may be in the best interest of child survival and safer to breastfeed.
During counselling on feeding options, you should cover the following:
- Discuss the advantages and disadvantages of each option;
- How to avoid breast problems/disease;
- How to use replacement feeding safely (mixing of milk, food hygiene);
- When and how to wean baby from breastfeeding;
- Appropriate complementary feeding for all infants.
- Follow up:
- All HIV exposed babies must be followed up until you can ensure that they are not infected by either doing the antibody test at 18 months or antigen test (PCR) any time before 18 months.
- Give cotrimoxazole prophylaxis to all exposed babies from age of 6 weeks until you prove that the baby is not infected.
- Continue counselling on feeding at each visit.
- Watch the growth curve – if the baby is not gaining weight appropriately despite nutrition counselling, the baby may have been HIV infected. Refer this baby to a facility that can carry out the tests to prove infection (PCR or CD4 counts).
If a child is proven to be infected refer to an appropriate centre for care.
- Immunisation:
Follow the national KEPI programme including the additional campaigns. Remember the caution on BCG, Some infected children may not show the scar on primary immunisation. Do not repeat BCG vaccination in this case as you may get a generalised reaction. If the child missed primary vaccines do these as soon as possible but avoid BCG if child is showing signs of AIDS infection.
- Give Vitamin A should be given according to national guidelines.
- Conduct Routine testing:
This can be in the antenatal clinic or children admitted to paediatric wards as well as all adults. The value of routine testing is to detect all infected parents and their children so that interventions can be instituted at the correct time. This would be the reverse of VCT. In fact some people call it DTC (Diagnosis, Testing and Counselling) or opt out. The country may be going this direction in future. The main drawback to this is the stigma attached to being HIV infected. Therefore you should ensure that you counsel and prepare the child and parents comprehensively if the results are positive.
SUMMARY
You have now come to the end of Unit 14 on HIV/AIDS in children. In this unit we discussed clinical presentation, diagnosis, treatment and management and how it can be prevented. There is a lot you can do to stop children from contracting the disease. There is also a lot you can do to manage and treat the infected ones effectively. But remember that this is a rapidly changing field. Care could change within days, weeks or months. So you need to keep up to date. Contact your DASCOP coordinator for current Ministry of Health guidelines from NASCOP.
Remember that children often get infected from parents. Ensure that the parents are also getting the care they need so that they can effectively look after their children.
PRACTICAL
- Find out where HIV programmes are in your district. Visit the site and learn more about comprehensive care of HIV infected people and PMTCT.
- For children attending clinic or admitted see if you can make a clinical diagnosis. Discuss these cases with your supervisor.
- In your station identify a pregnant HIV infected mother and participate in the care. Write a short brief of her history, diagnosis, and management including counselling. Submit the brief to your tutor before the end of this course.
- Explore how you can reduce stigma at the health facility and in the community.
Date
|
DIRECTORATE OF LEARNING SYSTEMS DISTANCE EDUCATION COURSES
Student Number: ________________________________ Name: _________________________________________ Address: _______________________________________ _______________________________________________
Unit 14: Assignment HIV/AIDS
1. Why is it difficult to diagnose HIV/AIDS in children? _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
_____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ 3. What are the common presentations of HIV/AIDS in children? _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
_____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
_____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ 6. Discuss the measures you would take to reduce stigma at your health facility and in the community. _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ Congratulations! You have now come to the end of this unit. Remember to indicate your Personal File Number, names and address before sending it.
|
Once you complete this assignment, post or bring it in person to AMREF Training Centre. We will mark it and return it to you with comments.
Our address is as follows:
Directorate of Learning Systems
AMREF Headquarters
P O Box 27691-00506
Nairobi, Kenya
Email: amreftraining@amrefhq.org